Ovarian Cycle and Hormonal Regulation
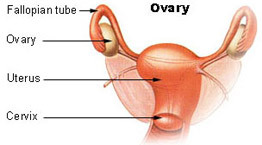
The ovarian cycle is a series of events in the ovaries that occur during and after the maturation of the oocyte (egg or ovum). During their reproductive years, nonpregnant females usually experience a cyclical sequence of changes in their ovaries and uterus. Each cycle takes about one month and involves both oogenesis, the process of formation and development of oocyte, and preparation of the uterus to receive a fertilized ovum. Hormones secreted by the hypothalamus, anterior pituitary gland, and ovaries control the principal events. The uterine (menstrual) cycle is a concurrent series of changes in the endometrium of the uterus to prepare it for the arrival of a fertilized ovum that will develop in the uterus until birth. If fertilization does not occur, the lining (stratum functionalis) of the endometrium is shed during menstruation. The general term female reproductive cycle encompasses the ovarian and uterine cycles, the hormonal changes that regulate them, and also the related cyclical changes in the breasts and cervix.
The ovarian and uterine cycles are controlled by chemical messengers or hormones. Gonadotropin releasing hormone (GnRH) is secreted by the hypothalamus and stimulates the release of follicle-stimulating hormone (FSH) and luteinizing hormone (LH) from the anterior pituitary gland. FSH, in turn, initiates follicular growth and the secretion of estrogens by the growth follicles. LH stimulates the further development of ovarian follicles and their full secretion of estrogens, brings about ovulation, promotes formation of the corpus luteum and stimulates the production of estrogens, progesterone, relaxin and inhibin by the corpus luteum.
Estrogens are hormones having several important functions. They promote the development and maintenance of female reproductive structures, secondary sex characteristics and the breasts. The secondary sex characteristics include the distribution of adipose tissue in the breasts, abdomen, and hips; also voice pitch, a broad pelvis and the pattern of hair growth on the head and body. Estrogens increase protein anabolism and lower blood cholesterol level. Moderate amount of estrogens in the body inhibit both the release of GnRH by the hypothalamus and secretion of LH and FSH by the anterior pituitary gland. At least six different estrogens are present in the plasma of human females but only three are present in significant quantities: B-estradiol, estrone, and estriol. In nonpregnant females, the principle estrogen is B-estradiol, which is synthesized from cholesterol in the ovaries.
Progesterone is secreted mainly by cells of the corpus luteum and acts synergistically with estrogens to prepare the endometrium for the implantation of a fertilized ovum and the mammary glands for milk secretion. High levels of progesterone also inhibit the secretion of GnRh and LH. A small quantity of the hormone relaxin produced by the corpus luteum during each monthly cycle, relaxes the uterus by inhibiting contractions. This is probably to facilitate the implantation of an ovum which is perhaps more likely to occur in a relaxed uterus. During pregnancy, the placenta produces much more relaxin and continues to relax the uterine smooth muscle. At the end of pregnancy, relaxin also increases the flexibility of the pubic symphysis and may help dilate the uterine cervix, both of which ease delivery of the baby. Inhibin is secreted by granulosa cells of growing follicles and by the corpus luteum of the ovary. It inhibits secretion of FSH and to a lesser extent, LH.
The duration of the reproductive cycle is divided into four phases: the menstrual phase, the preovulatory phase, ovulation, and the postovulatory phase. The menstrual phase lasts for about five days and by convention the first day of menstruation marks the first day of a new cycle. The endometrium is shed and the discharge occurs because the declining levels of hormones, especially progesterone, stimulating the release of prostaglandins that cause the uterine spiral arterioles to constrict. As a result the cells they supply become oxygen deprived and die and the stratum functionalis sloughs off. During this phase, some 20 secondary follicles in each ovary begin to enlarge and continue to do so through the preovulatory phase, the time between menstruation and ovulation, under the influence of FSH. By about day six, one follicle has outgrown the others and becomes the dominant follicle. Estrogens and inhibin secreted by the follicle decrease the secretion of FSH and the other follicles stop growing. The mature dominant follicle, or Graafian follicle, continues to enlarge until it is ready f or ovulation. It continues to produce estrogen under the influence of LH. At day 14, the follicle ruptures and releases an oocyte into the pelvic cavity. This process is known as ovulation. After ovulation the mature follicle collapses.
The postovulatory phase of the female reproductive cycle is the most constant in duration, lasting approximately from day 15 to 28 and represents the time between ovulation and the onset of the next menses. In the ovary, after ovulation, the LH stimulates the remnants of the mature follicle to develop into the corpus luteum, which secretes increasing quantities of progesterone and some estrogens. This is called the luteal phase of the ovarian cycle. Subsequent events in the ovary that ovulated an oocyte depend on whether or not the oocyte becomes fertilized. If the oocyte is not fertilized, the corpus luteum has a lifespan of only two weeks, after which it degenerates into a corpus albicans. As the levels of progesterone, estrogens, and inhibin decrease during this phase, GnRH, FSH, and LH release increases because of the lack of feedback suppression by the ovarian hormones. Then follicular growth resumes and a new ovarian cycle begins.
If, however, the oocyte is fertilized and begins to divide, the corpus luteum persists past its normal two-week lifespan. It is prevented from degenerating by the human chorionic gonadotropin (HCG), a hormone produced by the chorion of the embryo as early as eight to 12 days after fertilization. HCG acts like LH in stimulating the secretory activity of the corpus luteum and the presence of hCG in maternal blood or urine is an indicator of pregnancy.
See also Gamete; Gametogenesis; Reproductive system; Sexual reproduction.
Resources
Books
Adashi, E.Y. Ovulation: Evolving Scientific and Clinical Concepts. New York: Springer Verlag, 2000.
Grudzinskas, J.G., and J. Yovich, eds. Gametes: The Oocyte. Cambridge: Cambridge University Press, 1995.
Heffner, Linda G. Human Reproduction at a Glance. Oxford: Blackwell Science, 2001.
Judyth Sassoon
Additional topics
Science EncyclopediaScience & Philosophy: Octadecanoate to Ovenbirds